CHALLENGES
Diabetes poses numerous challenges in clinical practice. Some of those most commonly encountered include:
- High treatment costs. Diabetes is a progressive disease that requires ongoing intervention and, often, treatment intensification using combination therapy with 2 or more medications as the disease progresses. For some patients, the costs of increasing insurance premiums, deductibles, copays, and coinsurance are prohibitive.1
- Patient adherence. Cost of treatment, access to care, competing priorities, complicated treatment regimens and lack of disease awareness are frequently cited by patients as disincentives to adherence.1,2 Depression, stress, and fear of hypoglycemia or weight gain have also been shown to negatively impact patient adherence and diminish glycemic control.3,4
- Lack of disease intervention for prediabetes. According to the Centers for Disease Control and Prevention, 1 in 3 adults currently has prediabetes, and only 7% to 10% of them are aware of it. Without intervention, as many as 30% of people with prediabetes will develop type 2 diabetes within 3 years, placing a tremendous burden on individuals, society, and the healthcare system.1
- Poor coordination among healthcare providers. Electronic health information often is not easily retrievable, making it difficult for providers to identify patients with diabetes and track their multidisciplinary care.5
- Clinical inertia. Clinicians frequently do not respond promptly enough to evidence of poor glycemic control.6 Failure to intensify therapy in patients who have not met their glycemic goals can lead to persistent hyperglycemia, disease progression, and microvascular and macrovascular complications. Conversely, early, aggressive therapy intensification is associated with more rapid attainment of A1C goals and improved adherence. 7,8
Referral to appropriate resources for diabetes education, financial assistance, intensive behavioral counseling, and emotional support, as well as combination therapy to treat diabetes and comorbidities whenever appropriate, can aid clinicians and their patients with diabetes in overcoming many of these commonly encountered challenges, leading to more positive outcomes. In all cases, it is essential to engage patients as key stakeholders in their own care through shared decision-making and patient-centered, nonjudgmental communication.
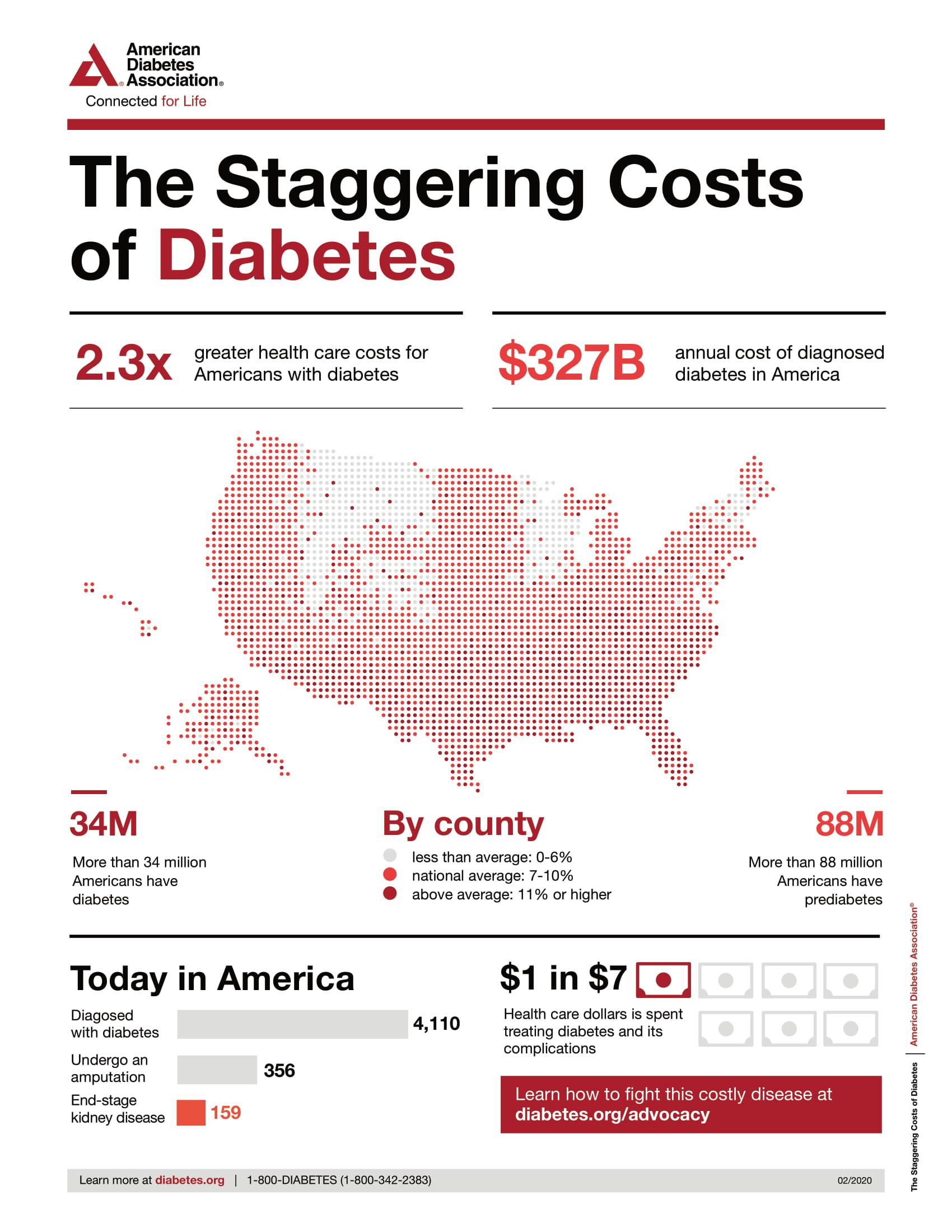
Source: ADA. https://www.diabetes.org/resources/statistics/cost-diabetes.
References
- Appold K. Four biggest challenges in diabetes health management. https://www.managedhealthcareexecutive.com/drug-pipeline/four-biggest-challenges-diabetes-health-management.
- García-Pérez L-E, et al. Adherence to Therapies in Patients with Type 2 Diabetes. Diabetes Ther. 2013;4(2):175-194.
- Badedi M, et al. Factors associated with long-term control of type 2 diabetes mellitus. J Diabetes Res. 2016;2016:2109542.
- Peyrot M, et al. Insulin adherence behaviours and barriers in the multinational Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabet Med. 2012;29(5):682-689.
- Appiah B, et al. Challenges and opportunities for implementing diabetes self-management guidelines. J Am Board Fam Med. 2013;26:90-92.
- Pantalone KM, et al. Clinical Inertia in Type 2 Diabetes Management: Evidence From a Large, Real-World Data Set. Diabetes Care. 2018;41(7):e113‐e114.
- Zonszein J, Groop PH. Strategies for diabetes management: using newer oral combination therapies early in the disease. Diabetes Ther. 2016;7:621-639.
- Bianchi C, et al. Early combination therapy with oral glucose-lowering agents in type 2 diabetes. Drugs. 2017;77:247-264.