Disadvantaged Populations
There are significant racial and ethnic disparities in diabetes prevalence and outcomes.1
- Hispanics, blacks, and Native Americans have a 50–100% greater burden of diabetes complications and mortality than whites.2
- At similar BMI levels, diabetes prevalence is higher in Asians than in whites.3
- Black patients are less likely to achieve treatment goals including glycemic, cholesterol, and blood pressure control.4
- Blacks experience worse long-term diabetes-related outcomes than whites, including diabetic retinopathy, lower-extremity amputations, and chronic kidney disease.4
- Native Americans experience disproportionately high rates of lower extremity amputations, chronic kidney disease, and diabetes-related mortality.4
- The prevalence of diagnosed diabetes among non-Hispanic black and Hispanic adults continues to increase but has leveled off among non-Hispanic whites.5
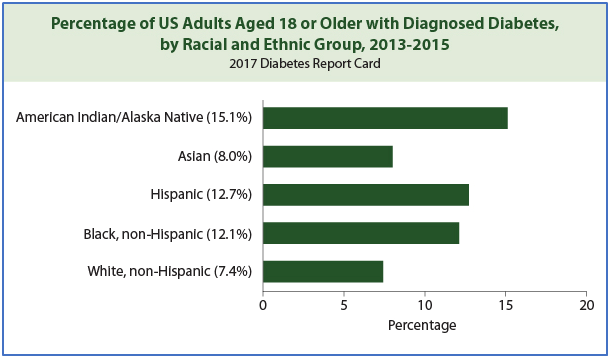
Source: Addressing Health Disparities in Diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/disparities.html.
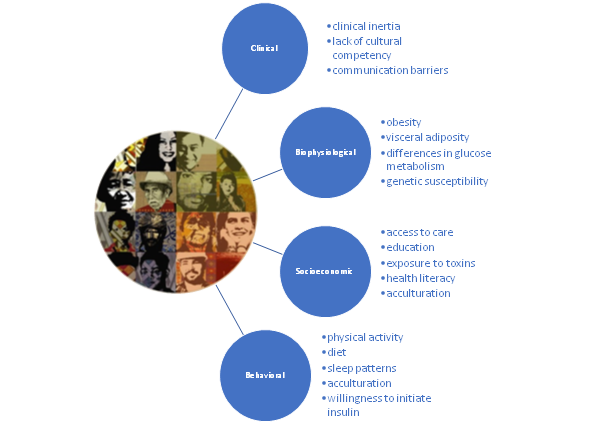
While the reasons are not yet completely understood, diabetes disparities probably result from complex interactions among clinical, biophysiological, socioeconomic, and behavioral factors.7
Contributors to Diabetes Health Disparities8–13
To improve health inequities related to diabetes, 2020 ADA Guidelines recommend that treatment be tailored for social context.
- Providers should assess social context, including potential food insecurity, housing stability, and financial barriers, and apply that information to treatment decisions.
- Refer patients to local community resources when available.
- Provide patients self-management support from lay health coaches, navigators, or community health workers when available.14
References
- Karter AJ, et al. Elevated Rates of Diabetes in Pacific Islanders and Asian Subgroups: The Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36(3):574-579.
- Canedo JR, et al. Racial/Ethnic Disparities in Diabetes Quality of Care: the Role of Healthcare Access and Socioeconomic Status. J Racial and Ethnic Health Disparities. 2018;5(1):7-14.
- Hsu WC, et al. BMI Cut Points to Identify At-Risk Asian Americans for Type 2 Diabetes Screening. Diabetes Care. 2015;38(1):150-158.
- Sequist TD, et al. Primary-care Clinician Perceptions of Racial Disparities in Diabetes Care. J Gen Intern Med. 2008;23(5):678-684.
- Beckles GL, Chou C-F. Disparities in the Prevalence of Diagnosed Diabetes – United States, 1999-2002 and 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65(45):1265-1269.
- Addressing Health Disparities in Diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/disparities.html.
- Dal Canto E. Why are there ethnic differences in cardio-metabolic risk factors and cardiovascular diseases? JRSM Cardiovasc Dis. 2018;7:2048004018818923.
- Peek ME, et al. Diabetes Health Disparities. Med Care Res Rev. 2007;64(5 Suppl):101S-156S.
- White RO, et al. Health Care Disparities and Diabetes Care: Practical Considerations for Primary Care Providers. Clinical Diabetes. 2009;27(3):105-112.
- Cook JP, Morris AP. Multi-ethnic genome-wide association study identifies novel locus for type 2 diabetes susceptibility. Eur J Hum Genet. 2016;24(8):1175-1180.
- Ruiz D, et al. Disparities in Environmental Exposures to Endocrine-Disrupting Chemicals and Diabetes Risk in Vulnerable Populations. Diabetes Care. 2018;41(1):193-205.
- Chatterjee R, et al. Novel Risk Factors for Type 2 Diabetes in African-Americans. CurrDiab Rep. 2015;15(12):103.
- Golden SH, et al. Health Disparities in Endocrine Disorders: Biological, Clinical, and Nonclinical Factors—An Endocrine Society Scientific Statement. J ClinEndocrinolMetab. 2012;97(9):E1579-E1639.
- American Diabetes Association. 1. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020; 43(Supplement 1):S7-S13.