SPECIAL POPULATION
Disadvantaged Populations
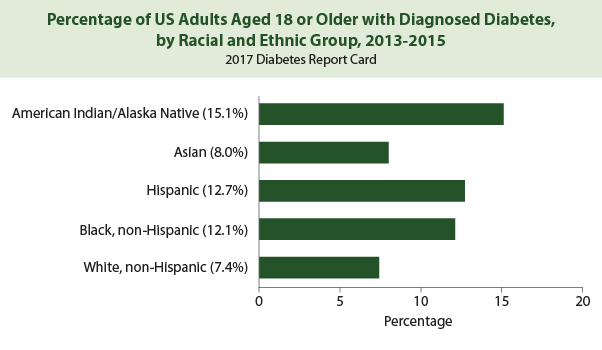
There are significant racial and ethnic disparities in diabetes prevalence and outcomes.1
- Hispanics, Blacks, and Native Americans have a 50–100% greater burden of diabetes complications and mortality than whites.2
- At similar BMI levels, diabetes prevalence is higher in Asians compared with whites.3
- Black patients are less likely to achieve treatment goals including glycemic, cholesterol, and blood pressure control.4
- Blacks experience worse long-term diabetes-related outcomes than whites, including diabetic retinopathy, lower extremity amputations, and chronic kidney disease.4
- Native Americans experiencing disproportionately high rates of lower extremity amputations, chronic kidney disease, and diabetes-related mortality.4
- The prevalence of diagnosed diabetes among non-Hispanic black and Hispanic adults continues to increase but has leveled off among non-Hispanic whites.5
Reference 1
While the reasons are not yet completely understood, diabetes disparities likely result from complex interactions between clinical, biophysiological, socioeconomic and behavioral factors.7
Contributors to Diabetes Health Disparities8–13

In order to improve health inequities related to diabetes, 2019 ADA Guidelines recommend that treatment be tailored for social context.
- Providers should assess social context, including potential food insecurity, housing stability, and financial barriers, and apply that information to treatment decisions.
- Refer patients to local community resources when available.
- Provide patients with self-management support from lay health coaches, navigators, or community health workers when available.14
References
- Karter AJ, Schillinger D, Adams AS, et al. Elevated Rates of Diabetes in Pacific Islanders and Asian Subgroups: The Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36(3):574-579. doi:10.2337/dc12-0722
- Canedo JR, Miller ST, Schlundt D, Fadden MK, Sanderson M. Racial/Ethnic Disparities in Diabetes Quality of Care: the Role of Healthcare Access and Socioeconomic Status. J Racial and Ethnic Health Disparities. 2018;5(1):7-14. doi:10.1007/s40615-016-0335-8
- Hsu WC, Araneta MRG, Kanaya AM, Chiang JL, Fujimoto W. BMI Cut Points to Identify At-Risk Asian Americans for Type 2 Diabetes Screening. Diabetes Care. 2015;38(1):150-158. doi:10.2337/dc14-2391
- Sequist TD, Ayanian JZ, Marshall R, Fitzmaurice GM, Safran DG. Primary-care Clinician Perceptions of Racial Disparities in Diabetes Care. J Gen Intern Med. 2008;23(5):678-684. doi:10.1007/s11606-008-0510-7
- Beckles GL, Chou C-F. Disparities in the Prevalence of Diagnosed Diabetes – United States, 1999-2002 and 2011-2014. MMWR Morb Mortal Wkly Rep. 2016;65(45):1265-1269. doi:10.15585/mmwr.mm6545a4
- Addressing Health Disparities in Diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/disparities.html. Published October 2, 2018. Accessed May 16, 2019.
- Dal Canto E, Farukh B, Faconti L. Why are there ethnic differences in cardio-metabolic risk factors and cardiovascular diseases? JRSM Cardiovasc Dis. 2018;7:2048004018818923. doi:10.1177/2048004018818923
- Peek ME, Cargill A, Huang ES. Diabetes Health Disparities. Med Care Res Rev. 2007;64(5 Suppl):101S-156S. doi:10.1177/1077558707305409
- White RO, Beech BM, Miller S. Health Care Disparities and Diabetes Care: Practical Considerations for Primary Care Providers. Clinical Diabetes. 2009;27(3):105-112. doi:10.2337/diaclin.27.3.105
- Cook JP, Morris AP. Multi-ethnic genome-wide association study identifies novel locus for type 2 diabetes susceptibility. Eur J Hum Genet. 2016;24(8):1175-1180. doi:10.1038/ejhg.2016.17
- Ruiz D, Becerra M, Jagai JS, Ard K, Sargis RM. Disparities in Environmental Exposures to Endocrine-Disrupting Chemicals and Diabetes Risk in Vulnerable Populations. Diabetes Care. 2018;41(1):193-205. doi:10.2337/dc16-2765
- Chatterjee R, Maruthur NM, Edelman D. Novel Risk Factors for Type 2 Diabetes in African-Americans. Curr Diab Rep. 2015;15(12):103. doi:10.1007/s11892-015-0675-5
- Golden SH, Brown A, Cauley JA, et al. Health Disparities in Endocrine Disorders: Biological, Clinical, and Nonclinical Factors—An Endocrine Society Scientific Statement. J Clin Endocrinol Metab. 2012;97(9):E1579-E1639. doi:10.1210/jc.2012-2043
- American Diabetes Association. 1. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S7-S12. doi:10.2337/dc19-S001
Older Adults
The natural history of diabetes in older adults differs from that in younger patients, due in part to shorter life expectancy, increased comorbidity and a greater risk of treatment-related complications.1
- 50-80% of adults >65 years of age have diabetes or prediabetes.2
- 61% of all expenditures attributed to diabetes are incurred by patients >65 years. 3
- Older adults with diabetes have higher complication rates than younger cohorts.3
- One-third of all individuals with diabetes are >65 years.4
Diabetes management strategies for high-functioning older people with a long life expectancy are similar to those used in younger patients.1 Life expectancy is an important factor in treatment decisions for older patients near the end of life. As morbidity and functional impairment increase, the anticipated benefit of glycemic control declines.2

Resources
References
- Strain WD, Hope SV, Green A, Kar P, Valabhji J, Sinclair AJ. Type 2 diabetes mellitus in older people: a brief statement of key principles of modern day management including the assessment of frailty. A national collaborative stakeholder initiative. Diabetic Medicine. 2018;35(7):838-845. doi:10.1111/dme.13644
- Halter JB, Musi N, Horne FM, et al. Diabetes and Cardiovascular Disease in Older Adults: Current Status and Future Directions. Diabetes. 2014;63(8):2578-2589. doi:10.2337/db14-0020
- Leung E, Wongrakpanich S, Munshi MN. Diabetes Management in the Elderly. Diabetes Spectrum. 2018;31(3):245-253. doi:10.2337/ds18-0033
- Schernthaner G, Schernthaner-Reiter MH. Diabetes in the older patient: heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61(7):1503-1516. doi:10.1007/s00125-018-4547-9
- American Diabetes Association. 12. Older Adults: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S139-S147. doi:10.2337/dc19-S012
Pregnant Women
The annual prevalence of pregestational diabetes is increasing, largely as a result of the obesity epidemic.1
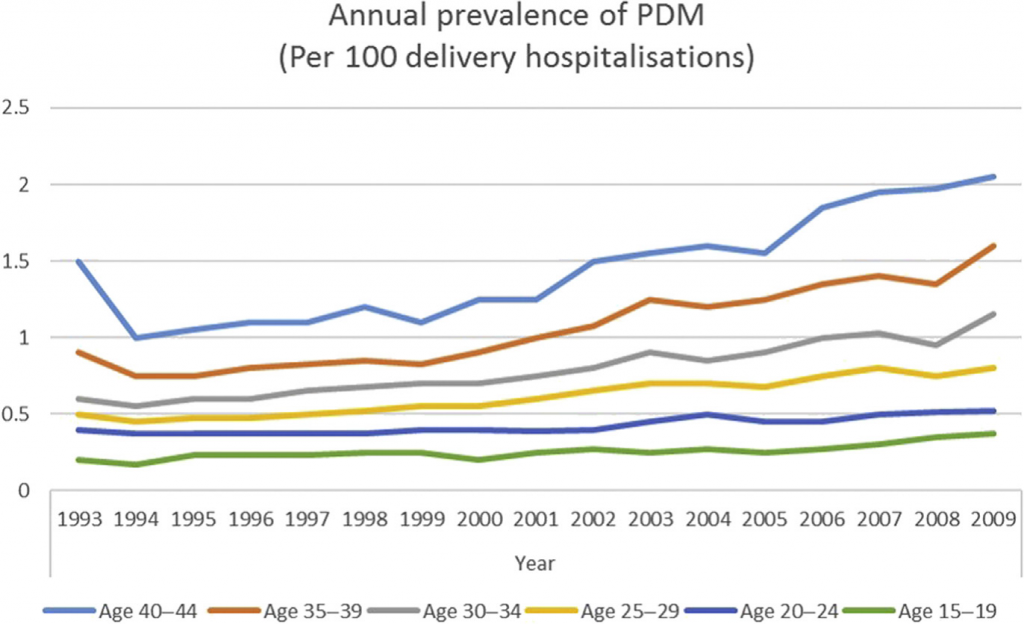
Reference 1
Adverse maternal and fetal consequences of poor glycemic control include2:
- congenital anomaly
- miscarriage
- pre-eclampsia
- pre-term delivery
- macrosomia
- stillbirth
- neonatal hypoglycemia.
Insulin is the preferred anti-hyperglycemic agent in pregnant women. Insulin requirements may change during pregnancy.3
[image5]
References:
- Sugrue R, Zera C. Pregestational Diabetes in Pregnancy. Obstet Gynecol Clin North Am. 2018;45(2):315-331. doi:10.1016/j.ogc.2018.01.002
- Etomi O, Banerjee A. The management of pre-existing (type 1 and type 2) diabetes mellitus in pregnancy. Medicine. 2018;46(12):731-737. doi:10.1016/j.mpmed.2018.09.004
- O’Neill SM, Kenny LC, Khashan AS, West HM, Smyth RM, Kearney PM. Different insulin types and regimens for pregnant women with pre-existing diabetes. Cochrane Database Syst Rev. 2017;2:CD011880. doi:10.1002/14651858.CD011880.pub2
- American Diabetes Association. 14. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2019. Diabetes Care. 2019;42(Supplement 1):S165-S172. doi:10.2337/dc19-S014
Resources:

Provider Toolkit

Challenges

Diagnosis

Epidemiology
Treatments