TREATMENTS
Diabetes has no cure. It is a chronic disease that requires life-long medical care paired with multifactorial strategies to reduce the risk of acute and serious long-term complications. Collaborating with patients to develop individualized management plans and glycemic targets and supporting their efforts to change behaviors are important components of improving outcomes.1
Lifestyle interventions include healthy eating, regular exercise, smoking cessation, weight management, and adopting strategies for coping with stress. Patients may need support with taking and managing medications; monitoring glucose levels and blood pressure; actively participating in screenings for eye, foot, and renal complications; adhering to the recommended immunization schedule; and identifying self-management problems and developing strategies to overcome them.1
Management plans should reflect key patient characteristics and specific factors that impact choice of treatment. A comprehensive medical evaluation should be conducted at diagnosis.1
Figure 1: Patient-centered management of type 2 diabetes2
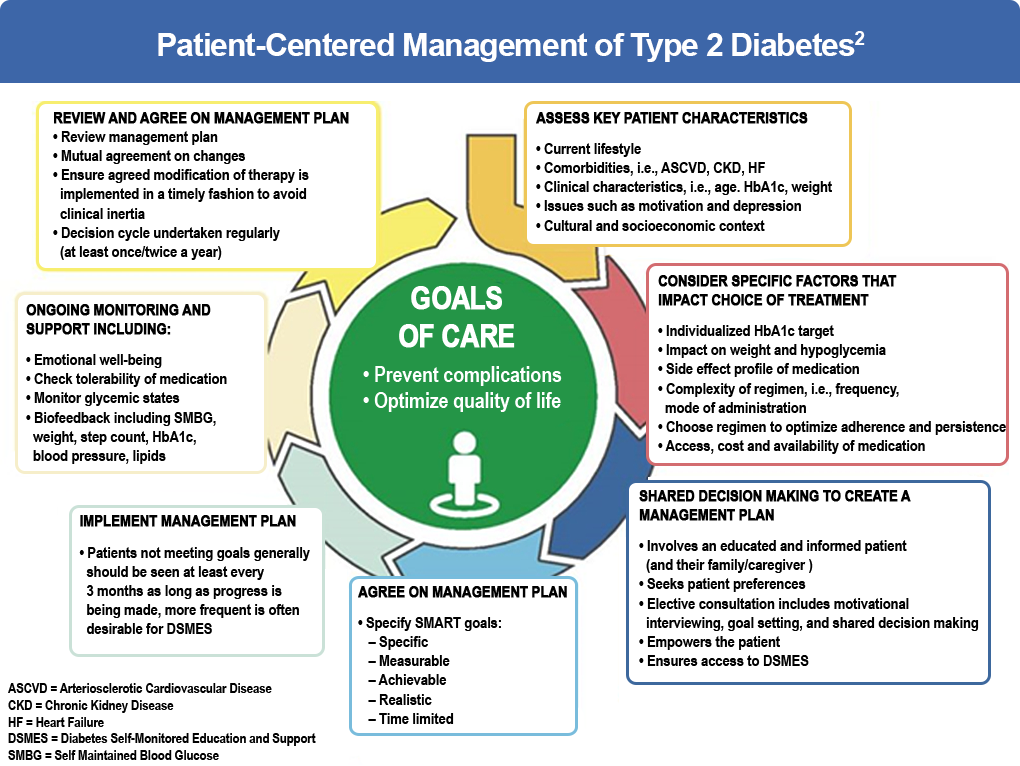
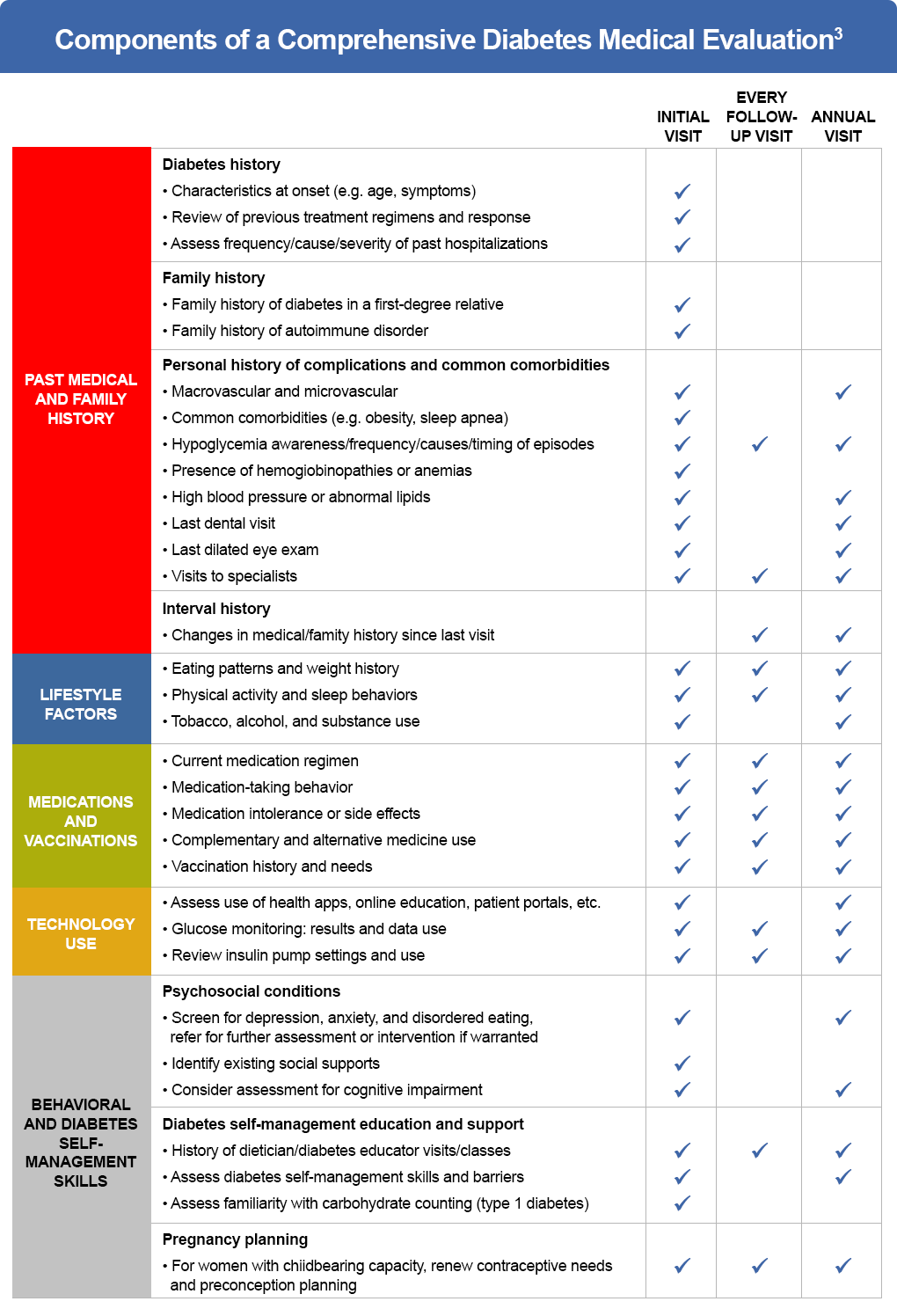
Figure 2: Components of a comprehensive diabetes medical evaluation3
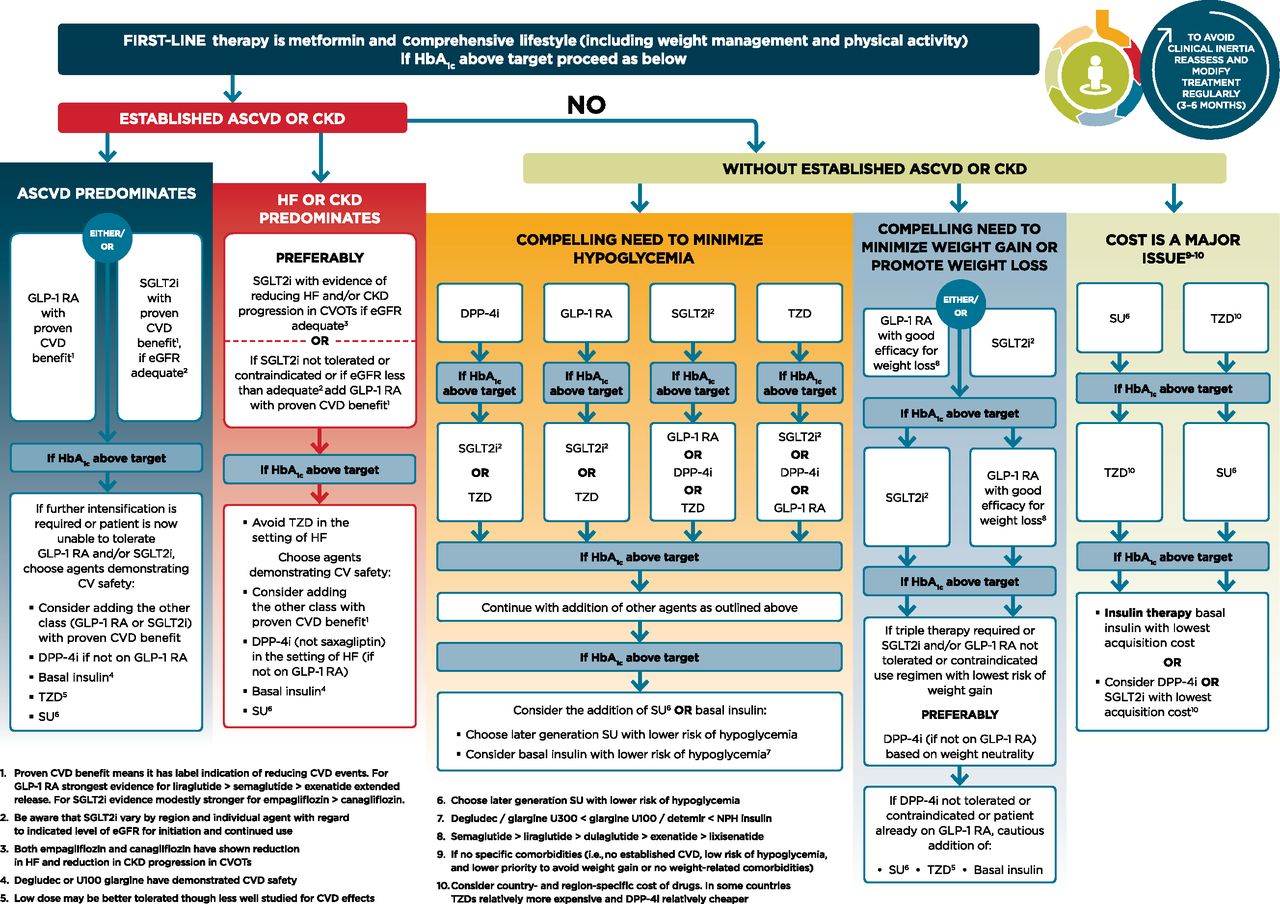
Unless there are contraindications, pharmacological treatment for patients with type 2 diabetes should begin with metformin at diagnosis. When metformin is contraindicated or if the patient cannot tolerate it, consideration should be given to a drug from another class, such as a sulfonylurea, thiazolidinedione, DPP-4 inhibitor, SGLT-2 inhibitor, GLP-1 receptor agonist, or insulin. Dual therapy should be considered for patients with newly diagnosed type 2 diabetes who have A1c ≥1.5% (12.5 mmol/mol) above their glycemic target. Insulin therapy should be considered when blood glucose is ≥300 mg/dL (16.7 mmol/L), A1c is ≥10% (86 mmol/mol), or if the patient has symptoms of hyperglycemia (ie, polyuria or polydipsia), even at diagnosis or early in treatment. 1
The 2021 ADA Standards of Medical Care in Diabetes recommend a patient-centered approach to treatment selection that factors in comorbidities (atherosclerotic cardiovascular disease, heart failure, chronic kidney disease), hypoglycemia risk, impact on weight, cost, risk for side effects, and patient preferences.1
Figure 3: Considering patient-specific factors in treatment selection1
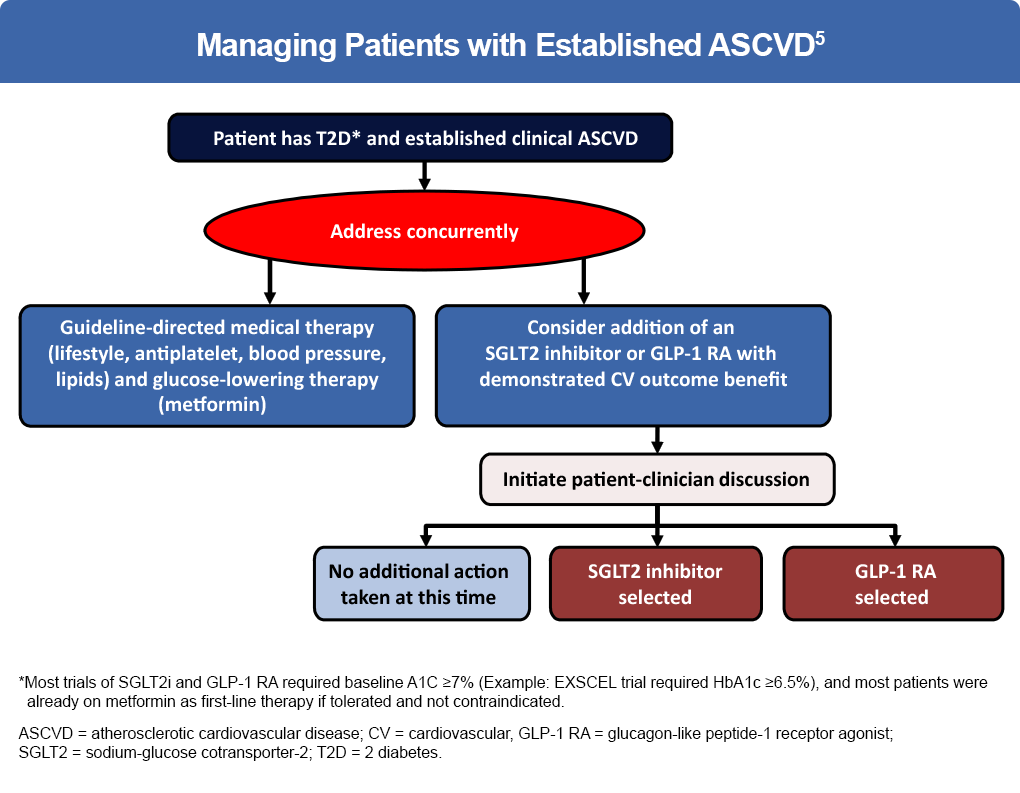
The prevention of adverse cardiovascular outcomes is a key component of diabetes management.
- Among patients with type 2 diabetes older than 65 years, atherosclerotic CVD (ASCVD) accounts for up to 70% of deaths3
- Diabetes-related ASCVD results in an estimated $37.3 billion in cardiovascular-related spending per year.4
- Rates of incident heart failure hospitalization are two-fold higher in patients with diabetes than in those without.5
Treatment with statins, aspirin, glucose-lowering therapies, and blood pressure reduction should be considered on a background of intensive lifestyle management including exercise, nutrition, and weight management in all patients with type 2 diabetes.5
Selecting medications solely for their potential to lower hemoglobin A1c is an outdated therapeutic approach. The recent development of 2 novel classes of therapies —GLP-1RAs and SGLT2 inhibitors — has provided evidence that treatments developed for glucose lowering can directly improve cardiovascular outcomes.
Figure 4: Managing patients with established ASCVD5
Complete guidelines for diabetes treatment can be found at:
- American Diabetes Association. Standards of Medical Care in Diabetes—2021: https://care.diabetesjournals.org/content/suppl/2020/12/09/44.Supplement_1.DC1
- AACE/ACE Comprehensive Type 2 Diabetes Management Algorithm (2020) – EXECUTIVE SUMMARY: https://www.aace.com/disease-state-resources/diabetes/clinical-practice-guidelines-treatment-algorithms/comprehensive
References
- American Diabetes Association. Standards of Medical Care in Diabetes—2020 Abridged for Primary Care Providers. Clin Diabetes. 2020;38(1):10-38.
- Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Cares. 2018;41:2669-2701.
- Pasquel FJ, et al. The evolving epidemiology of atherosclerotic cardiovascular disease in people with diabetes. Endocrinol Metab Clin North Am. 2018;47(1):1-32.
- American Diabetes Association. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes—2020. Diabetes Care. 2020; 43 (suppl 1):S111-S134.
- Newman JD, et al. Primary prevention of cardiovascular disease in diabetes mellitus.
J Am Coll Cardiol. 2017;70(7):883-893. - Das SR, et al. 2018 ACC expert consensus decision pathway on novel therapies for cardiovascular risk reduction in patients with type 2 diabetes and atherosclerotic cardiovascular disease: A report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;72(24):3200‐3223.